Preparing for Allergies and Asthma During Emergencies
In today's unpredictable world, being prepared for emergencies is more important than ever, especially for those who suffer from allergies and asthma. Imagine being caught in a natural disaster or a sudden crisis, and your breathing becomes labored, or you break out in hives. It’s a nightmare scenario, but with the right strategies in place, you can navigate these situations more safely. This article discusses essential strategies for managing allergies and asthma in emergency situations, ensuring safety and preparedness for individuals who suffer from these conditions.
Allergies and asthma are not just seasonal nuisances; they are serious conditions that can significantly impact your quality of life. Allergies occur when your immune system reacts to a foreign substance, such as pollen, pet dander, or certain foods. Symptoms can range from mild sneezing and itching to severe reactions that require immediate medical attention. On the other hand, asthma is a chronic condition that affects the airways, making them inflamed and narrow, which can lead to difficulty breathing. During emergencies, the stress and environmental changes can exacerbate these conditions, making it crucial to understand their triggers and symptoms.
Developing a personalized emergency action plan is crucial for individuals with allergies and asthma. This plan should include specific steps to take during an emergency, ensuring that you can act quickly and effectively. Consider the following key components:
- Emergency Contacts: List family members, friends, and healthcare providers who should be contacted in case of an emergency.
- Medication List: Keep a detailed list of your medications, including dosages and instructions, and ensure you have a supply readily available.
- Emergency Procedures: Outline what to do if you experience an allergic reaction or asthma attack, including when to seek medical help.
Recognizing specific allergens and asthma triggers is vital for effective management. Common triggers include:
- Pollen from trees, grasses, and weeds
- Dust mites and mold spores
- Smoke from fires or cigarettes
- Strong odors from perfumes or cleaning products
During emergencies, it’s essential to minimize exposure to these triggers. For example, if you know a storm is coming, try to stay indoors and keep windows closed to limit pollen and dust entry.
Environmental factors such as pollen, dust, and smoke can worsen symptoms. Here are some strategies to reduce exposure:
- Stay indoors during high pollen counts or air quality alerts.
- Use air purifiers to filter out allergens in your home.
- Wear a mask if you must go outside during an emergency that could stir up dust or smoke.
Food allergies can pose serious risks during emergencies, especially if you are in an unfamiliar setting. To avoid food allergens, always:
- Read labels carefully, even on packaged foods.
- Communicate your allergies clearly when eating out or in communal settings.
- Carry your own allergen-free snacks to ensure you have safe options available.
Proper medication management is essential for individuals with allergies and asthma. Ensure that you have quick access to your medications, including rescue inhalers and antihistamines. Consider organizing a medication kit that includes:
- Rescue inhalers
- Antihistamines
- Any other prescribed medications
Store these medications in a waterproof container and keep them with you during emergencies to avoid any delays in treatment.
An effective emergency supplies checklist can significantly improve safety. Make sure to include essential items for managing allergies and asthma during crises. Here’s a quick rundown:
- Essential Medications: Rescue inhalers, antihistamines, and any prescribed medications.
- Other Necessary Supplies: Masks to filter out allergens, allergen-free snacks, and a first-aid kit.
Clear communication with emergency personnel is vital. When you encounter first responders, ensure they are aware of your allergies and asthma. Carrying a medical alert card can help convey this information quickly and effectively, allowing for appropriate care.
Educating those around you about your allergies and asthma can enhance safety. Share your emergency action plan with family and friends, and ensure they know how to assist you during an emergency. The more they understand, the better support you’ll receive when it matters most.
Recovery after an emergency is crucial for individuals with allergies and asthma. After the dust settles, take the time to assess your health and well-being. Follow up with your healthcare provider to ensure your treatment plan is still effective, and make adjustments as necessary. This proactive approach can help you regain your footing and stay healthy in the aftermath of any crisis.
Q: What should I do if I experience an asthma attack during an emergency?
A: Use your rescue inhaler immediately and try to remain calm. If symptoms persist, seek medical help as soon as possible.
Q: How can I ensure my family understands my allergies?
A: Have open discussions about your allergies, provide them with written information, and practice scenarios where they need to help you.
Q: What items should I include in my emergency kit?
A: Include essential medications, a first-aid kit, masks, allergen-free snacks, and a list of emergency contacts.

Understanding Allergies and Asthma
Allergies and asthma are two common conditions that can significantly impact a person's quality of life. Understanding what they are, their causes, and their symptoms is essential for effective management, especially in emergency situations. Allergies occur when the immune system reacts to foreign substances, known as allergens, which can be anything from pollen and dust mites to certain foods and medications. This reaction can lead to symptoms such as sneezing, itching, and difficulty breathing, making everyday activities challenging.
On the other hand, asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to wheezing, coughing, chest tightness, and shortness of breath. While asthma can be triggered by various factors, including allergens, respiratory infections, and exercise, it is crucial to recognize that emergencies can exacerbate both allergies and asthma symptoms. For instance, during a natural disaster, increased stress levels, changes in the environment, and limited access to medications can lead to severe asthma attacks or allergic reactions.
It's important to note that allergies and asthma often coexist, and individuals with allergies are at a higher risk of developing asthma. The interplay between these conditions can complicate management and increase the likelihood of emergency situations. Therefore, understanding the specific triggers and symptoms of both conditions is vital. Here are some common triggers:
- Environmental Triggers: Pollen, dust, mold, and pet dander.
- Food Allergens: Nuts, shellfish, dairy, and gluten.
- Weather Changes: Extreme temperatures and humidity levels.
- Stress and Anxiety: Emotional stress can trigger asthma attacks.
Recognizing these triggers and their potential to worsen symptoms during emergencies can help individuals take proactive measures to avoid exposure. For example, staying indoors during high pollen counts or having an emergency kit ready with necessary medications can be lifesaving. In addition, understanding the symptoms of an allergic reaction or an asthma attack can help individuals respond quickly and effectively when faced with an emergency.
Ultimately, the key to managing allergies and asthma lies in education and preparedness. By familiarizing oneself with the conditions, recognizing triggers, and having a solid plan in place, individuals can navigate emergencies with greater confidence and safety.

Creating an Emergency Action Plan
When it comes to managing allergies and asthma during emergencies, having a well-structured Emergency Action Plan is not just a good idea—it's essential. Think of it as your personal roadmap to safety, guiding you through the chaos and uncertainty that can arise in critical situations. So, what exactly should this plan entail? Let’s break it down into manageable components that will keep you prepared and calm, even when the unexpected hits.
First and foremost, your action plan should include a clear outline of your allergies and asthma triggers. This is crucial because knowing what can provoke your symptoms allows you to avoid those triggers as much as possible during an emergency. For instance, if you are allergic to pollen, you might want to stay indoors during a high pollen count day or seek shelter in a less exposed area. Documenting these triggers not only helps you but also informs anyone who might assist you in an emergency, such as family members or first responders.
Next, consider incorporating a section that details your medication regimen. This includes the names of your medications, dosages, and the frequency with which you take them. You might want to create a simple table for this information to make it easy to read at a glance. Here’s a quick example of how you might structure it:
| Medication | Dosage | Frequency |
|---|---|---|
| Rescue Inhaler | 90 mcg | As needed |
| Antihistamine | 10 mg | Once daily |
Additionally, your plan should include emergency contact information. This not only encompasses family members but also your healthcare provider and any specialists who might need to be contacted in a crisis. Make sure this information is readily accessible—consider keeping a copy in your wallet or on your phone. You can even share it with a trusted friend or neighbor who can step in to help if you’re unable to communicate your needs.
Another critical element of your action plan is to outline the steps to take in case of an emergency. This could mean having a list of symptoms that indicate you need to take action, such as using your rescue inhaler or taking an antihistamine. For instance, if you start experiencing wheezing, shortness of breath, or swelling, your plan should clearly state what you should do next. This clarity can make a world of difference when time is of the essence.
Lastly, it’s important to regularly review and update your action plan. Life changes, and so do your health needs. Whether it’s a new medication, a change in your allergies, or even a move to a different environment, keeping your plan current ensures that you’re always prepared. Set a reminder every few months to go over your plan, make necessary adjustments, and keep everyone informed.
By taking the time to create a comprehensive Emergency Action Plan, you empower yourself to manage your allergies and asthma effectively, even in the face of emergencies. Remember, preparation is the key to safety, and your plan is your safety net.
Q: How often should I review my Emergency Action Plan?
A: It's advisable to review your plan every few months or whenever there is a significant change in your health or living situation.
Q: What should I do if I experience an allergic reaction during an emergency?
A: Follow the steps outlined in your action plan, including using your rescue inhaler or antihistamines, and seek help immediately if symptoms worsen.
Q: Can I share my Emergency Action Plan with others?
A: Absolutely! Sharing your plan with family, friends, and caregivers ensures that they know how to assist you in an emergency.

Identifying Triggers
When it comes to managing allergies and asthma, is like finding the key to a locked door. Knowing what sets off your symptoms can make all the difference in staying safe, especially in emergency situations. Triggers can vary widely from person to person, but they generally fall into a few common categories. Understanding these can help you not only recognize but also avoid them whenever possible.
One of the most prevalent triggers for asthma and allergies is environmental factors. These include things like pollen, dust mites, mold, and pet dander. For those with seasonal allergies, pollen can be a significant issue, particularly during spring and fall. Imagine waking up on a beautiful spring day, only to be greeted by a sneeze and itchy eyes the moment you step outside. To combat this, it’s essential to monitor pollen counts and stay indoors when levels are high. Additionally, keeping windows closed and using air purifiers can help minimize exposure.
Another major category is food allergens. For individuals with food allergies, even a tiny crumb can lead to a severe reaction. Common culprits include peanuts, tree nuts, dairy, and shellfish. The challenge often arises during emergencies, like when you're at a shelter or a friend's house, where food options may be limited or unknown. Always read labels and ask about ingredients, because being in a rush doesn’t exempt you from the risk of an allergic reaction.
It's also important to note that stress and anxiety can act as triggers for asthma symptoms. In a chaotic situation, like a natural disaster or an unexpected emergency, your body might react by tightening airways, leading to an asthma attack. This is why having a plan in place to manage stress is crucial. Techniques such as deep breathing exercises or having a calming item, like a favorite book or photo, can help mitigate these effects.
To better illustrate the types of triggers you might encounter, consider the following table:
| Trigger Type | Examples | Management Strategies |
|---|---|---|
| Environmental | Pollen, Dust, Mold, Pet Dander | Stay indoors, use air purifiers, and keep windows closed. |
| Food | Peanuts, Tree Nuts, Dairy, Shellfish | Read labels, ask about ingredients, and carry safe snacks. |
| Stress | Emotional distress, anxiety | Practice deep breathing, keep calming items on hand. |
In summary, identifying your triggers is the first step in creating a safe environment, especially during emergencies. By understanding what can provoke your allergies or asthma, you can take proactive measures to avoid these situations. Remember, knowledge is power! The more you know about your triggers, the better equipped you’ll be to handle any emergency that comes your way.

Environmental Triggers
When it comes to managing allergies and asthma, can be sneaky little devils. They lurk in the air we breathe and can turn an ordinary day into a struggle for breath and comfort. Understanding these triggers is essential, especially during emergencies when your usual coping mechanisms might be compromised.
Common environmental triggers include pollen, dust mites, mold, and smoke. Imagine stepping outside on a beautiful spring day, only to be ambushed by a cloud of pollen from blooming trees and flowers. For someone with allergies, that’s like walking into a war zone. And don’t even get me started on dust mites—they're like tiny ninjas hiding in your bedding, waiting to strike when you least expect it. During emergencies, such as natural disasters, these triggers can become even more prevalent due to displaced debris and changes in living conditions.
So, how can you minimize your exposure to these environmental hazards during a crisis? Here are some practical strategies:
- Stay Indoors: Whenever possible, remain indoors during high pollen counts or when air quality is poor. Use air conditioning to keep your living space cool and filter out allergens.
- Seal Windows and Doors: In case of smoke or dust storms, ensure that windows and doors are tightly sealed to prevent outdoor pollutants from entering your home.
- Use Air Purifiers: Investing in a good air purifier can help reduce indoor allergens significantly. Look for models with HEPA filters for the best results.
- Wear Masks: If you must go outside, consider wearing a mask designed to filter out allergens. This can be particularly useful during wildfires or high pollen seasons.
Additionally, it's crucial to stay informed about the air quality in your area. Many apps and websites provide real-time updates on pollen counts and air quality indices. By keeping tabs on this information, you can plan your activities accordingly and avoid unnecessary exposure to harmful triggers.
In summary, being aware of environmental triggers and taking proactive steps to mitigate their effects can make all the difference for individuals with allergies and asthma, especially during emergencies. Remember, preparation is key. Just like you wouldn’t go into battle without your armor, don’t face environmental challenges without a solid plan in place!
Q: What are the most common environmental triggers for asthma and allergies?
A: The most common environmental triggers include pollen, dust mites, mold, pet dander, and smoke. Each of these can provoke symptoms and lead to serious complications if not managed properly.
Q: How can I prepare my home for allergy season?
A: Regular cleaning, using air purifiers, and keeping windows closed during high pollen counts can help reduce allergens in your home. Additionally, consider using hypoallergenic bedding to minimize dust mites.
Q: What should I do if I have an asthma attack during an emergency?
A: Use your rescue inhaler as prescribed, and try to move to a less polluted area if possible. If symptoms persist, seek medical attention immediately.
Q: Are there any specific masks that can help with allergies?
A: Masks labeled as N95 or higher can filter out small particles, including pollen and dust, making them effective for individuals with allergies.

Food Allergens
When it comes to emergencies, food allergens can be a silent yet deadly threat for individuals with allergies. Imagine being in a chaotic situation, perhaps at a shelter or during a community event, and suddenly encountering a food item that could trigger a severe reaction. The anxiety this can cause is palpable. To navigate these treacherous waters, it’s essential to be proactive and informed about potential food allergens.
First and foremost, understanding what constitutes a food allergen is critical. Common food allergens include:
- Peanuts
- Tree nuts
- Shellfish
- Fish
- Milk
- Eggs
- Soy
- Wheat
These foods are notorious for causing reactions ranging from mild hives to severe anaphylaxis. Knowing these allergens can empower you to make safer choices during emergencies.
One of the best strategies to avoid food allergens is to always read labels. In emergency situations, food may be distributed without clear labeling, so it’s vital to ask questions. If you’re unsure about an ingredient, it’s better to err on the side of caution and avoid the food altogether. Additionally, consider packing your own snacks that you know are safe. This way, you can ensure you have allergen-free options available, reducing the risk of exposure.
Another important aspect to consider is cross-contamination. This occurs when allergenic foods come into contact with safe foods, often in shared cooking or serving environments. For instance, if someone prepares a meal with peanuts and then uses the same utensils for a dish meant for you, the risk of an allergic reaction increases significantly. To mitigate this risk, be vocal about your allergies and request that your food be prepared separately.
In situations where food is being served, such as at shelters or community gatherings, it’s wise to have a food allergy action plan. This plan should include:
- Emergency contacts
- Your specific allergens
- Signs of an allergic reaction
- Steps to take in case of exposure
By having a clear plan, you can communicate effectively with those around you, ensuring they understand the gravity of your situation.
Lastly, always carry an epinephrine auto-injector if you have a history of severe reactions. This device can be a lifesaver in emergencies, providing immediate relief until professional medical help can be obtained. Make sure that your family and friends are aware of where you keep it and how to use it. It’s not just a personal safety measure; it’s a community effort.
In conclusion, being prepared for food allergens during emergencies is not just about knowledge; it’s about action. By understanding your allergens, reading labels, avoiding cross-contamination, and having a solid action plan, you can significantly reduce the risks associated with food allergies. Remember, preparedness is your best defense!
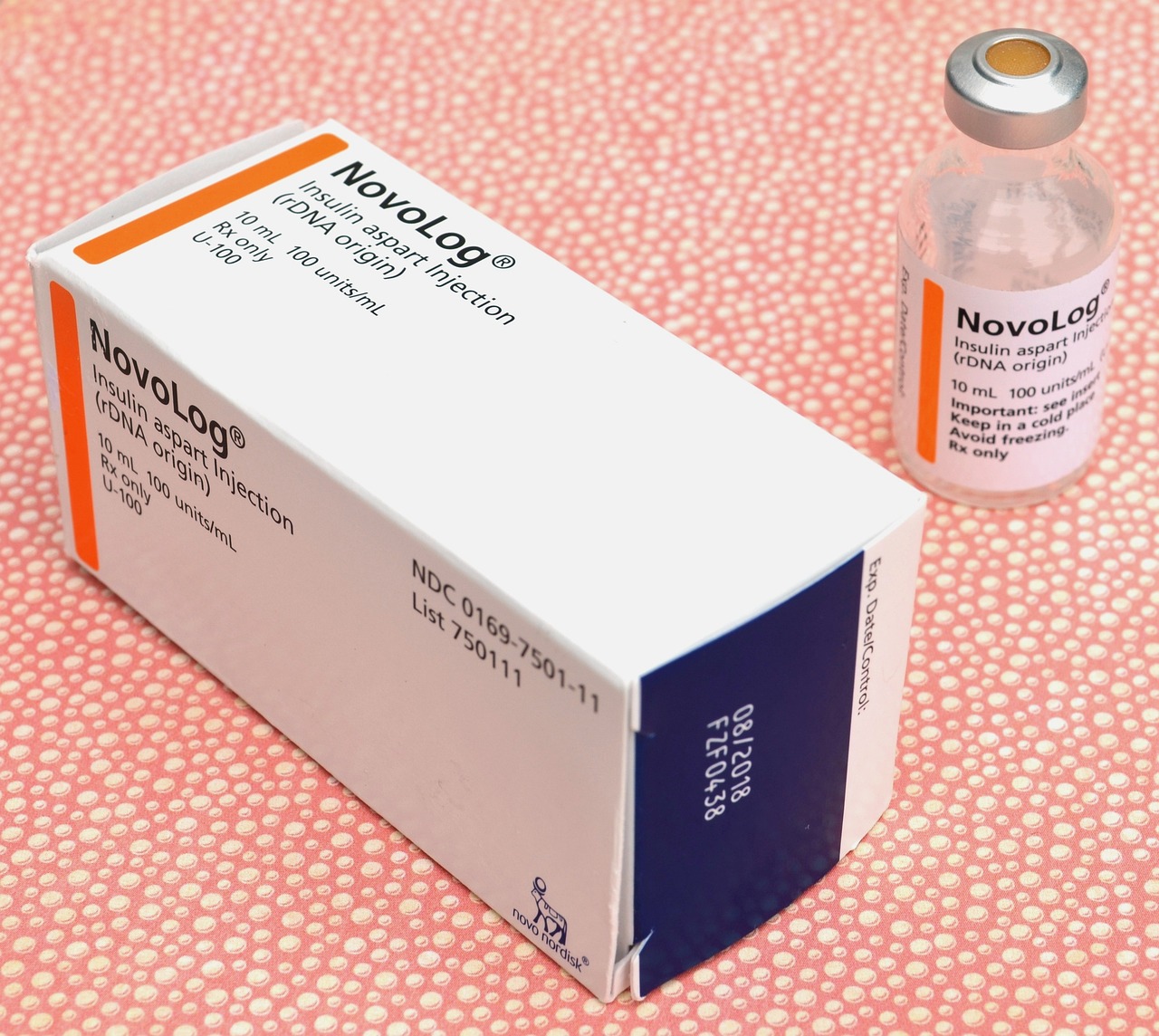
Medication Management
When it comes to managing allergies and asthma, is not just important; it's essential. Imagine being in an emergency situation where your symptoms flare up, and you can't find your rescue inhaler or antihistamines. The panic that follows can be overwhelming. That's why having a well-thought-out plan for your medications is crucial. Start by making a comprehensive list of all your necessary medications, including dosages and instructions. This list should be easily accessible, whether it's in your wallet, on your phone, or posted on your fridge.
It's also wise to keep a supply of your medications in a designated emergency kit. This kit should include not only your prescribed medications but also any over-the-counter remedies that you might need, such as antihistamines for allergic reactions. Make sure to check the expiration dates regularly, as expired medications can be ineffective when you need them most. Furthermore, consider keeping a copy of your prescriptions in your emergency kit. This can be incredibly helpful if you need to refill your medications in an unfamiliar location.
Another vital aspect of medication management is understanding how to use your medications correctly. For instance, if you have an inhaler, ensure that you know the proper technique to maximize its effectiveness. If you're unsure, consult your healthcare provider for a demonstration. You might also want to practice using your inhaler or any other devices in a calm setting, so when an emergency arises, you can act swiftly and efficiently.
Communication is key when it comes to medication management. Make sure that your family and friends are aware of your medications, including how and when to administer them. This ensures that they can assist you in case of an emergency. You might even consider creating a simple chart that outlines your medications, dosages, and administration times. This can be a lifesaver during a stressful situation.
Lastly, always keep your medications in a safe and secure location. If you're traveling or evacuating, ensure that you have your medications packed and ready to go. Using a waterproof bag can protect your medications from damage. Remember, being prepared is half the battle when it comes to effectively managing allergies and asthma during emergencies.
- What should I include in my emergency medication kit? Your kit should include all prescribed medications, over-the-counter antihistamines, a copy of your prescriptions, and any necessary medical devices like inhalers or epinephrine auto-injectors.
- How often should I check my medication expiration dates? It's best to check your medication expiration dates at least every six months to ensure you have effective medications when you need them.
- Can my family help me manage my medications? Absolutely! Educating your family and friends about your medications can be incredibly beneficial. They can assist you during emergencies by knowing what to do and when to act.

Emergency Supplies Checklist
When it comes to managing allergies and asthma during emergencies, having an can be a lifesaver. Think of it as your personal toolkit, ready to tackle any unexpected situation that might arise. You wouldn't head out on a road trip without packing snacks and a spare tire, right? Similarly, being prepared with the right supplies can make all the difference when the unexpected strikes.
First and foremost, it's crucial to have a list of essential medications at your fingertips. This includes not only your daily medications but also any rescue inhalers and antihistamines. Imagine being caught in a situation where your asthma flares up, and you can't find your inhaler—it's a nightmare scenario. To prevent that, make sure to have at least two rescue inhalers on hand, especially if you’re going to be in an area where you might encounter allergens or irritants.
Additionally, consider the environmental triggers that could exacerbate your condition. For example, if you're heading into a crowded place, a simple face mask can help filter out dust and allergens. Keeping a few disposable masks in your emergency kit is a great way to minimize exposure. Also, don't forget to include allergen-free snacks in your supplies. During emergencies, food options may be limited, and having safe snacks can help you avoid accidental exposure to food allergens.
Here’s a quick overview of what your emergency supplies checklist should include:
| Item | Description |
|---|---|
| Rescue Inhalers | Always carry at least two for emergencies. |
| Antihistamines | Over-the-counter options can help with allergic reactions. |
| Face Masks | To reduce exposure to airborne allergens. |
| Allergen-Free Snacks | To avoid accidental exposure during stressful situations. |
Moreover, don’t overlook other necessary supplies that can enhance your preparedness. Having a first-aid kit that includes allergy-specific supplies, such as an epinephrine auto-injector for severe allergic reactions, can be invaluable. And if you have specific triggers, like pet dander or mold, consider including items like air purifiers or cleaning wipes to help manage your environment.
Finally, remember that being prepared isn’t just about having the right items; it’s also about knowing how to use them. Familiarize yourself with your medications and their dosages, and practice using your auto-injector if you have one. It’s like learning to ride a bike; the more you practice, the more confident you’ll feel when it’s time to put that knowledge into action.

Essential Medications
When it comes to managing allergies and asthma during emergencies, having the right medications on hand can make all the difference. Imagine being in a situation where you can’t breathe or are faced with a severe allergic reaction. It’s a nightmare scenario, but with proper preparation, you can navigate these challenges more effectively. First and foremost, it’s crucial to carry your rescue inhaler. This small device is a lifesaver for individuals with asthma, providing quick relief from sudden symptoms. Always ensure that your inhaler is easily accessible, whether you’re at home or out and about.
In addition to your rescue inhaler, it’s wise to have a supply of antihistamines on hand. These medications can help alleviate symptoms associated with allergies, such as sneezing, itching, and hives. During emergencies, you may encounter allergens that you don’t typically face, so being prepared with antihistamines can help you manage unexpected reactions. It’s also beneficial to have a plan for storing these medications. Consider using a waterproof pouch or a dedicated medication bag to keep them safe and organized.
Another essential component of your emergency medication kit is a steroid inhaler. While not everyone with asthma requires this, for those who do, having it readily available can prevent a serious situation from escalating. Steroid inhalers work by reducing inflammation in the airways, providing longer-term control of asthma symptoms. If you’re unsure about what medications are necessary for your specific condition, it’s best to consult with your healthcare provider.
To help you visualize these essential medications, here’s a quick table summarizing their importance:
| Medication Type | Purpose |
|---|---|
| Rescue Inhaler | Provides immediate relief from asthma symptoms |
| Antihistamines | Alleviates allergy symptoms |
| Steroid Inhaler | Reduces inflammation in airways for long-term control |
Always remember to check the expiration dates on your medications regularly. An expired inhaler or antihistamine can be ineffective when you need it the most. Also, consider carrying a medication list that includes dosages and instructions. This list can be invaluable in emergency situations, especially when communicating with first responders. By being prepared and organized, you can significantly reduce the stress associated with managing allergies and asthma during emergencies.
In summary, the right medications are your first line of defense against allergy and asthma emergencies. Whether it’s a rescue inhaler, antihistamines, or a steroid inhaler, having these essentials at your fingertips can provide peace of mind and a sense of control during chaotic moments. So, take the time to gather and organize your medications, and ensure that you and your loved ones are ready for anything that comes your way.
- What should I do if my inhaler is lost during an emergency? - Try to remain calm and seek immediate assistance from emergency personnel or a nearby pharmacy for a replacement.
- How often should I check my medication supplies? - It’s a good idea to check your supplies at least once a month, especially before entering allergy or asthma season.
- Can I carry my medications in my purse or backpack? - Yes, just ensure they are stored in a waterproof pouch to protect them from moisture.

Other Necessary Supplies
When it comes to managing allergies and asthma during emergencies, having the right supplies on hand can make all the difference. Beyond just medications, there are several essential items that can help you navigate through crises more safely. Think of it as packing a safety net; it’s not just about having your rescue inhaler or antihistamines, but also about being prepared for various situations that can arise.
First and foremost, consider carrying masks. These can be particularly useful in environments where air quality may be compromised, such as during wildfires or dust storms. A mask can help filter out harmful particles, thus reducing the risk of triggering an asthma attack. Look for masks that are designed to filter out particulate matter, such as N95 respirators, which can provide a higher level of protection.
Another critical item to include in your emergency kit is allergen-free snacks. If you have food allergies, it’s essential to have safe options readily available. Being caught in a situation where food is scarce or potentially unsafe can heighten anxiety and put your health at risk. Stock up on snacks that you know are safe for you, such as:
- Rice cakes
- Nut-free granola bars
- Dried fruits
- Vegetable chips
Additionally, don’t forget about saline nasal sprays. These can help alleviate nasal congestion that may arise from allergens or irritants in the environment. Keeping your nasal passages clear can be particularly beneficial in preventing asthma symptoms from escalating. A small bottle can easily fit into your emergency bag without taking up much space.
Furthermore, having a portable air purifier can be a game-changer, especially in enclosed spaces. These devices can help filter out allergens and pollutants from the air, providing a cleaner environment. If you’re in a situation where you have to stay indoors, an air purifier can significantly improve air quality, allowing you to breathe easier.
Lastly, consider including a first-aid kit that specifically addresses your needs. This kit should not only contain general supplies like band-aids and antiseptic wipes but also specific items related to your allergies and asthma. For example, include an extra epinephrine auto-injector if you have severe allergies, as well as a list of your allergies and emergency contacts. This way, if you are incapacitated, someone else can provide the necessary information to first responders.
In conclusion, being prepared for emergencies involves more than just medications. By packing these additional supplies, you can create a comprehensive plan that not only addresses your immediate health needs but also provides peace of mind. After all, preparation is key to handling unexpected situations with confidence.
Q: What should I include in my emergency kit for allergies and asthma?
A: Your emergency kit should include essential medications, masks, allergen-free snacks, saline nasal sprays, a portable air purifier, and a personalized first-aid kit tailored to your specific needs.
Q: How can I reduce exposure to allergens during an emergency?
A: To minimize exposure, use masks to filter air, stay indoors when possible, and utilize air purifiers to improve air quality. Always have your medications on hand in case of an allergic reaction or asthma attack.
Q: Why is it important to educate family and friends about my allergies and asthma?
A: Educating those around you ensures they understand your conditions and can assist you in emergencies. They will know how to react and what to do if you experience a severe allergic reaction or asthma attack.

Communication with First Responders
When emergencies strike, the last thing you want is to be fumbling for words or information about your allergies and asthma. Clear communication with first responders can be a game changer, and it’s essential for ensuring that you receive the appropriate care. Imagine being in a situation where every second counts—having a plan in place to convey your medical needs can make all the difference.
First and foremost, it's crucial to have a medical ID that clearly states your allergies and asthma condition. This could be a bracelet or a card that you carry in your wallet. When first responders arrive, they often have to make quick decisions, and a medical ID can provide them with critical information at a glance. But what if you don’t have your ID on you? That’s where it becomes important to be prepared with a quick summary of your medical history.
When speaking to first responders, try to be as concise and clear as possible. Here are some key points to convey:
- Your medical conditions: Clearly state that you have allergies and asthma.
- Specific triggers: Mention any known triggers that may worsen your condition, like certain foods, pollen, or smoke.
- Current medications: Inform them about the medications you are currently taking, especially rescue inhalers or antihistamines.
- Severity of symptoms: Describe how you are feeling, whether you are experiencing mild discomfort or severe symptoms.
Additionally, if you have family or friends with you, encourage them to speak up as well. They can provide valuable information that you might forget in the heat of the moment. It’s like having a safety net—someone there to back you up when you need it most.
In some cases, first responders may not be familiar with specific allergies or asthma management protocols. It’s important to remember that they are trained to handle emergencies, but they may not know every nuance of your condition. Therefore, being proactive and providing them with as much information as possible is vital. If you have an action plan or a list of medications, don’t hesitate to share that with them. It can help them make informed decisions about your care.
Lastly, always keep your contact information for your healthcare provider handy. If first responders need to consult with a doctor about your condition, having that information readily available can expedite the process. Think of it as having your own personal emergency hotline!
In conclusion, effective communication with first responders is not just about stating facts; it’s about empowering yourself and ensuring that you receive the best possible care in an emergency. The more prepared you are, the better your chances of staying safe and healthy, even in the most chaotic situations.
Q1: What should I include in my medical ID for allergies and asthma?
A1: Your medical ID should include your name, allergies, asthma condition, and any critical medications you take. This information helps first responders act quickly.
Q2: How can I prepare my family for emergencies related to my allergies and asthma?
A2: Educate your family about your conditions, including triggers and emergency actions. Practice scenarios together so they know what to do if an emergency arises.
Q3: What if I am unable to communicate during an emergency?
A3: Having a medical ID and an emergency action plan can help communicate your needs even if you cannot speak. Ensure that your family knows where to find this information.

Educating Family and Friends
When it comes to managing allergies and asthma, having a solid support system is absolutely essential. Imagine navigating a stormy sea without a life raft—this is often how individuals with these conditions feel without the backing of family and friends. Educating those around you about your specific allergies and asthma can significantly improve your safety and well-being during emergencies. So, how can you effectively share this critical information? Let's dive in!
First off, it’s important to have an open and honest conversation with your family and friends. Start by explaining your condition in simple terms. You might say something like, “I have asthma, which means I can have trouble breathing if I’m exposed to certain triggers, like smoke or strong scents.” This straightforward approach helps demystify your condition and makes it easier for them to understand the seriousness of the situation.
Next, consider creating an allergy and asthma information sheet. This document should include:
- Your specific allergies and asthma triggers.
- Signs and symptoms of an asthma attack or allergic reaction.
- Emergency contact information, including your doctor’s number.
- Instructions on how to use your medications, like inhalers or EpiPens.
Having this information readily available can be a lifesaver, especially in high-pressure situations. Place copies of the sheet in common areas, like the fridge or near the first aid kit, so that they can easily access it when needed.
It's also wise to conduct a few practice drills. Just like fire drills in schools, these practice runs can help your loved ones feel more prepared and confident in handling a real emergency. Role-play different scenarios where they might need to assist you, whether it’s recognizing the signs of an allergic reaction or knowing how to administer your medications. This hands-on approach not only reinforces their understanding but also builds a sense of teamwork and preparedness.
Lastly, encourage your family and friends to ask questions. A simple “What do you want me to do if you have an asthma attack?” can open the door to a deeper conversation. This not only shows that they care but also ensures they fully grasp the importance of your condition. Remember, knowledge is power, and the more informed your support system is, the better equipped they will be to help you in times of need.
In summary, educating your family and friends about your allergies and asthma is a proactive step towards ensuring your safety. By sharing information, conducting practice drills, and fostering open communication, you can create a network of support that makes navigating emergencies a little less daunting. After all, in the face of adversity, having a solid support system can make all the difference!
Q: How can I convince my family to take my allergies seriously?
A: Share personal experiences and explain the potential consequences of exposure to allergens. Providing educational materials can also be helpful.
Q: What should I do if someone around me doesn't understand my condition?
A: Have a calm conversation, explaining your triggers and symptoms. Offer to provide written information they can refer to.
Q: How can I educate my children about my allergies?
A: Use simple language and relatable examples. Role-play scenarios where they might need to help you, reinforcing their understanding.
Post-Emergency Recovery
After the storm has passed, the dust has settled, and the chaos of an emergency situation is behind you, it's time to focus on recovery. This phase is crucial, especially for those managing allergies and asthma, as your body needs to recuperate, and you need to ensure that your environment is safe for your health. Just like a flower needs sunlight and water to bloom again after a harsh winter, you too need to nurture your well-being following an emergency.
The first step in the recovery process is to assess your health. Take note of any symptoms that may have surfaced during the emergency. Did you experience increased wheezing, shortness of breath, or allergic reactions? Documenting these symptoms can help you and your healthcare provider understand the impact of the emergency on your condition. It’s like keeping a diary of your health; the more you write, the clearer the picture becomes.
Next, it's vital to re-establish a safe environment. This may involve cleaning your living space to remove any allergens that may have accumulated during the emergency. For instance, if you were exposed to dust or mold, a thorough cleaning with HEPA filters can significantly improve air quality. Consider this step as creating a sanctuary, a safe haven where you can breathe easy and relax.
Don't forget to review and replenish your emergency supplies. After an emergency, it’s common for medications and supplies to be depleted. Check your stock of rescue inhalers, antihistamines, and any other necessary medications. Think of it as restocking your toolbox; you wouldn’t want to start a project without the right tools at hand!
Moreover, follow up with your healthcare provider. Schedule an appointment to discuss any health changes you experienced during the emergency. This is also a great opportunity to review your allergy and asthma management plan. Your doctor can provide tailored advice to help you bounce back stronger, ensuring that you are equipped to handle any future emergencies more effectively.
Lastly, don’t underestimate the power of support systems. Reach out to family and friends to share your experiences and feelings. They can provide emotional support and help you navigate the recovery process. Just like a team of firefighters working together to extinguish a blaze, your loved ones can help you overcome the aftermath of an emergency.
In summary, post-emergency recovery is not just about physical health; it’s about emotional and mental well-being too. By taking proactive steps to assess your health, create a safe environment, replenish supplies, consult with healthcare providers, and lean on your support network, you can ensure a smoother recovery process. Remember, recovery is a journey, not a race, so take it one step at a time.
- What should I do if I experience an asthma attack after an emergency? - Use your rescue inhaler immediately and seek medical attention if symptoms persist.
- How can I ensure my home is allergen-free after an emergency? - Regular cleaning, using air purifiers, and ensuring proper ventilation can help reduce allergens.
- Should I change my medication routine after an emergency? - Consult with your doctor to determine if any changes are necessary based on your post-emergency health status.
Frequently Asked Questions
- What should I include in my emergency action plan for allergies and asthma?
Your emergency action plan should include a list of your specific allergies and asthma triggers, a detailed medication list, and instructions on what to do in case of an allergic reaction or asthma attack. Make sure to share this plan with family and friends so they can assist you if needed.
- How can I identify my allergy and asthma triggers?
Identifying your triggers involves paying attention to your symptoms and the environments in which they worsen. Common environmental triggers include pollen, dust, and smoke, while food allergens can vary widely. Keeping a journal of your symptoms can help pinpoint specific triggers more effectively.
- What essential medications should I have during an emergency?
It’s crucial to have your rescue inhaler, antihistamines, and any other prescribed medications readily available. Always keep them in an accessible location, and consider carrying a spare set in your emergency kit to ensure you’re prepared for any situation.
- How can I communicate my allergies and asthma to first responders?
When communicating with first responders, be clear and concise. Use simple language to describe your allergies and asthma, and inform them about your emergency action plan. If possible, carry a medical alert card that lists your conditions and medications to make it easier for them to assist you.
- What are some tips for educating my family and friends about my allergies and asthma?
Start by having open conversations about your conditions, explaining what triggers your allergies and asthma, and outlining what they should do in an emergency. Consider providing them with written information or resources that they can refer to in case of an emergency.
- How can I recover effectively after an emergency related to my allergies or asthma?
Post-emergency recovery involves monitoring your symptoms closely and following up with your healthcare provider. Take time to rest, re-evaluate your emergency action plan, and ensure you have all necessary medications stocked and ready for future situations.